No te pierdas la transmisión en vivo.
CONVERSATORIO
SABER QUE MORIRÁ SUFRIENDO
10 DE ABRIL, 5:00 PM
También puedes seguir la transmisión en los siguientes canales de DMD México.

DMD MÉXICO
Por El Derecho a Morir con Dignidad
Cuidados Paliativos Muerte Medicamente Asistida Dignidad Post Mortem
DMD INICIA UNA NUEVA ETAPA
DMD amplía su campo de trabajo para contribuir a garantizar el derecho a un proceso de final de vida digno y sin sufrimiento.
El derecho a morir con dignidad incluye la capacidad de decidir la forma en que deseamos ser cuidados en el proceso final de la vida.
Ampliamos nuestro campo de trabajo a tres ejes:
- Cuidados paliativos.
- Muerte médicamente asistida.
- Cuidados post mortem.
Información y Documentación

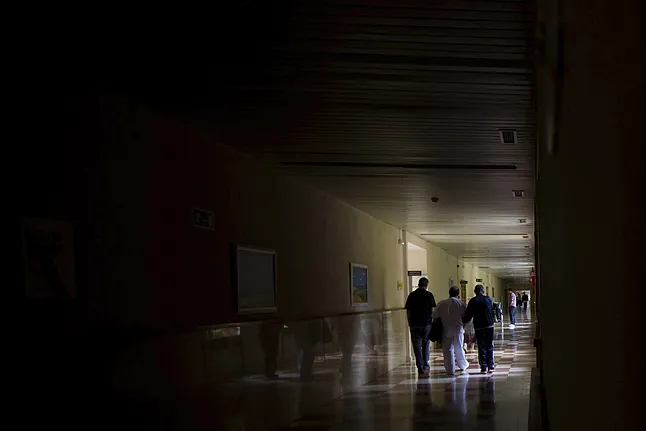
Cuidados Paliativos
Contribuyen a mejorar la calidad de vida de los pacientes y de sus familias, cuando afrontan enfermedades graves, progresivas e incurables y que limitan su esperanza de vida.

Voluntad Anticipada
Documento escrito que contiene la manifestación de una persona sobre sus preferencias respecto a los cuidados y tratamientos de salud que desea recibir en el proceso del final de la vida.
Estos deben cumplirse en el momento en que no tenga la capacidad para expresarlas personalmente.

Muerte Médicamente Asistida
En México, actualmente la ley no permite practicar la eutanasia o el suicidio asistido, sin embargo, se está avanzando.
DMD ha contribuido a abrir el debate y en la actualidad hay una iniciativa de ley en el Congreso de la Unión.

Toma de Decisiones
En ocasiones, nos enfrentamos a situaciones que nos generan un dilema ético, es decir, debemos elegir entre opciones que tienen consecuencias positivas y negativas al mismo tiempo. No necesariamente hay un respuesta correcta o incorrecta. Los dilemas éticos plantean un conflicto de valores y principios. Estas situaciones merecen una reflexión.

Información al Paciente
El paciente tiene derecho a recibir la información y participar en la toma de decisiones en los temas relativos a su salud.
El principio de “autonomía“ es el fundamento de los derechos de los pacientes

Cuidados Post-Mortem
Los cuidados y preparación post-mortem son esenciales para honrar la memoria y el legado de aquellos que han partido.
Estas prácticas buscan preservar la dignidad del fallecido, al mismo tiempo que proporcionan un apoyo necesario para los seres queridos en un momento de duelo.